Foot Pain Slowing You Down? Safe Therapy to Help You Move Comfortably
Foot pain making walking difficult? Learn how physical therapy helps. Get expert care at HWY Physical Therapy Clinic in Salem, OR.
Learn the symptoms and treatment options for nerve damage from diabetes. HWY Physical Therapy Clinic in Salem, OR helps improve balance and mobility.
Nerve damage from diabetes is a common condition, but many people do not notice it until symptoms start to interfere with daily life. High blood sugar can slowly damage nerves, most often in the feet and legs, leading to pain, numbness, tingling, or balance problems.
These changes usually develop gradually and may worsen over time if they are not addressed. Many people dismiss early symptoms, assuming they are just part of getting older.
For adults 50 and older, diabetic nerve damage can increase the risk of falls, foot injuries, and loss of independence. Early action can make a meaningful difference. With the right treatment and guidance, many people are able to reduce symptoms, improve mobility, and stay active. For those living in Salem, Oregon, understanding the signs and available care options is an important first step.
Nerve damage from diabetes, also called diabetic neuropathy, happens when high blood sugar levels injure nerves over time. This condition most often affects the feet and legs, but it can also impact the hands, digestive system, heart, and other areas.
Diabetic neuropathy is one of the most common complications of diabetes. Many people have some level of nerve damage before they realize it, especially if symptoms start mild.
Nerves help the body feel pain, temperature, and pressure. They also control muscle movement and automatic functions like digestion and blood flow.
When nerves are damaged, these signals do not travel properly between the body and the brain. This can lead to pain, numbness, weakness, or loss of coordination.
High blood sugar can damage the small blood vessels that supply nerves. When nerves do not get enough oxygen and nutrients, they begin to malfunction.
Over time, repeated blood sugar spikes cause inflammation and breakdown of the nerve covering. This slows nerve signals and reduces sensation.
Diabetic neuropathy does not always mean permanent nerve loss. In many cases, symptoms can be slowed, stabilized, or improved with early care.
While damaged nerves may not fully heal, proper treatment can reduce pain and help preserve function. Acting early gives the best chance of protecting mobility and independence.
Diabetes causes nerve damage when high blood sugar stays elevated for long periods. Excess sugar in the bloodstream interferes with how nerves send signals and how they receive nourishment.
Nerves rely on healthy blood vessels to deliver oxygen and nutrients. Diabetes can damage these small vessels, which slowly starves the nerves and weakens their function.
High blood sugar creates chemical changes inside nerve cells. These changes reduce the nerves’ ability to repair themselves and protect their outer coating.
Over time, nerve signals slow down or misfire. This is why people may feel burning, tingling, or numbness even without an obvious injury.
People who have lived with diabetes for many years face a higher risk of nerve damage. Poor circulation also increases the likelihood of nerve problems.
Adults over 50 are more vulnerable due to natural changes in blood flow and nerve health. A less active lifestyle can make symptoms progress faster.
Unstable blood sugar levels place constant stress on nerves. Smoking further reduces circulation and oxygen delivery.
Foot injuries that go unnoticed can worsen nerve damage. Without early care, these factors can speed up symptom progression.

Early nerve damage from diabetes often starts with subtle changes that are easy to overlook. Many people mistake these signs for normal aging or circulation issues.
Common early symptoms include tingling or pins-and-needles sensations in the toes or feet. Numbness may come and go, especially after sitting or lying down.
Some people notice a mild burning feeling, often worse at night. Others feel increased sensitivity, where light touch or bedsheets feel uncomfortable.
Cold or hot sensations without a clear reason can also be an early warning sign. Balance may feel slightly off, even without noticeable weakness.
Catching these symptoms early matters. Addressing nerve changes at this stage can help slow progression and protect long-term mobility.
As nerve damage from diabetes progresses, symptoms often become more noticeable and harder to ignore. These symptoms can vary from person to person and may change over time.
Many people experience ongoing numbness or reduced feeling in the feet. This can make it harder to notice cuts, blisters, or pressure points.
Tingling or buzzing sensations may feel mild at first. Occasional sharp or stabbing pains can come and go without warning.
Some people notice changes in how their feet sense temperature. Walking may feel different, even though strength seems normal.
Loss of sensation in the feet can interfere with balance and walking. Muscle weakness may develop, increasing the risk of trips and falls.
Pain may become constant and interfere with sleep. Simple activities like standing for long periods can feel exhausting.
Nerve pain often feels stronger at night because there are fewer distractions. Circulation changes during rest can also heighten nerve sensitivity.
When the body slows down, damaged nerves may send stronger pain signals. This can make burning or aching sensations more noticeable after bedtime.
Diabetic neuropathy is not a single condition. Diabetes can damage different types of nerves, which explains why symptoms vary so widely from person to person.
Understanding the type of neuropathy involved helps guide treatment and daily management.
Peripheral neuropathy is the most common form of diabetic nerve damage. It usually affects the feet, toes, and legs first, and sometimes the hands.
Symptoms may include numbness, burning pain, tingling, or weakness. Balance problems and difficulty walking often develop as sensation decreases.
Autonomic neuropathy affects nerves that control automatic body functions. These include digestion, blood pressure, heart rate, and bladder control.
People may notice dizziness when standing, digestive discomfort, or changes in sweating. These symptoms can be subtle and are often missed early.
Proximal neuropathy causes pain and weakness in the hips, thighs, or buttocks. It often affects one side of the body and can make standing or walking difficult.
Focal neuropathy involves sudden damage to a specific nerve. This may cause sharp pain or weakness in the face, torso, or leg.
Nerve damage from diabetes is diagnosed through a combination of symptom review and physical testing. Early diagnosis helps reduce the risk of complications like falls and foot injuries.
A healthcare provider will often ask about pain, numbness, balance issues, and changes in sensation. These details help determine how nerves may be affected.
Simple tests are commonly used to check nerve function. These may include light touch, vibration, temperature, and reflex testing.
Providers also examine muscle strength and coordination. Changes in balance or walking patterns can point to nerve involvement.
You should seek help if numbness, tingling, or pain becomes persistent. Loss of sensation in the feet is another important warning sign.
Sudden weakness, frequent falls, or foot wounds that heal slowly should be addressed right away. Early evaluation allows treatment to begin before nerve damage worsens.
Treatment for nerve damage from diabetes focuses on reducing symptoms and slowing further nerve injury. Most treatment plans combine medical care with lifestyle and movement-based strategies.
Managing blood sugar levels is a critical first step. Consistent blood sugar control helps limit ongoing nerve stress and supports overall nerve health.
Medications are often used to reduce nerve pain. These may help with burning, tingling, or shooting sensations.
While medications can ease discomfort, they do not repair damaged nerves. Relying on medication alone may leave balance, strength, and movement issues unaddressed.
Non-drug approaches focus on improving how nerves communicate with muscles and the brain. These therapies aim to support function rather than only mask pain.
Movement-based care, balance training, and neuromuscular re-education are becoming more common. Technology-assisted options are also being explored, including methods designed to help the nervous system relearn proper signaling.
Some people seek additional education on advanced neuropathy approaches, such as those discussed at https://www.neu.fit/neuropathy/. Learning about emerging options can help individuals make informed decisions alongside professional guidance.

Physical therapy can play an important role in managing diabetic nerve damage. It focuses on improving how the body moves, balances, and responds to nerve signals.
Rather than treating pain alone, physical therapy addresses the physical changes caused by nerve damage. This approach helps people move with more confidence and control.
Nerve damage in the feet can make balance less reliable. Physical therapy helps retrain balance through guided exercises and safe movement practice.
Strengthening the legs and core improves stability while walking. This reduces the risk of falls, which is especially important for adults 50 and older.
Targeted exercises help improve coordination between nerves and muscles. Over time, this can lead to better movement awareness and control.
Therapy also supports circulation, which is essential for nerve health. Improved blood flow can help reduce stiffness and discomfort.
As we age, nerve recovery becomes more challenging. Physical therapy helps maintain independence by improving strength, mobility, and balance.
For many people, staying active safely is key to long-term quality of life. Physical therapy provides structure and guidance to support that goal.
Living with nerve damage from diabetes can be frustrating, especially when symptoms begin to affect balance, walking, or daily comfort. Having access to local care makes it easier to get consistent support and guidance.
People in Salem, Oregon do not need to manage diabetic neuropathy alone. Targeted care can help reduce fall risk, improve movement, and support long-term independence.
HWY Physical Therapy provides one-on-one care focused on function, safety, and confidence. Treatment plans are personalized to address balance issues, strength loss, and movement changes caused by nerve damage.
Rather than relying only on pain relief, care is designed to help people move better and feel more stable in daily life. This approach is especially helpful for adults managing long-term diabetes.
Care at HWY Physical Therapy is led by Dr. Raj, who works closely with adults age 50 and older. Treatment is provided at the Center 50+ in the Salem City Building, making access convenient and supportive.
Patients receive clear guidance, hands-on care, and progress tracking throughout treatment. To schedule an appointment or learn more, call 971-202-1979.
Slowing nerve damage from diabetes starts with daily habits that protect nerve health. Small, consistent changes can help reduce symptoms and prevent further progression.
Natural strategies work best when combined with professional care. These steps support the nervous system and overall mobility.
Keeping blood sugar levels stable reduces stress on nerves. Large swings in blood sugar can speed up nerve damage.
Regular monitoring, balanced meals, and staying hydrated all support nerve function. Consistency matters more than perfection.
Daily foot checks help catch small problems before they become serious. Numbness can make cuts or pressure spots easy to miss.
Wearing supportive footwear protects sensitive areas and improves stability. Proper foot care lowers the risk of infections and balance issues.
Regular movement improves blood flow to the nerves. Gentle walking, stretching, and guided exercise can help maintain sensation and strength.
Staying active also supports balance and confidence. Movement is one of the most effective natural tools for protecting nerve health.

Living with nerve damage from diabetes can affect both physical comfort and emotional well-being. Daily pain, numbness, or balance issues can make routine tasks feel more difficult.
Many people feel frustrated when symptoms limit activities they once enjoyed. Learning how to manage these changes can help restore a sense of control.
Chronic nerve pain can be unpredictable. Some days may feel manageable, while others feel more challenging.
Developing consistent routines, staying active within safe limits, and seeking professional guidance can help reduce stress. Support and education play an important role in coping with long-term symptoms.
Staying active helps protect strength, balance, and confidence. Even small amounts of regular movement can improve daily function.
Simple adjustments, such as using supportive footwear or modifying activities, can make a big difference. The goal is to stay as independent and mobile as possible while protecting nerve health.
Can nerve damage from diabetes be reversed?
Diabetic nerve damage cannot always be fully reversed, but symptoms can often be slowed or improved. Early treatment, blood sugar control, and movement-based care can help protect remaining nerve function.
Does diabetic neuropathy always get worse?
Diabetic neuropathy does not always worsen if it is managed early. Many people are able to stabilize symptoms and maintain mobility with consistent care and healthy habits.
Is walking good or bad for diabetic neuropathy?
Walking is usually helpful when done safely. Gentle, regular walking improves circulation, supports balance, and helps maintain strength, which benefits nerve health.
When should I see a physical therapist for diabetic nerve damage?
You should consider physical therapy if you notice balance issues, weakness, frequent falls, or changes in how you walk. Early support can improve safety and help you stay active longer.
If nerve damage from diabetes is affecting your balance, comfort, or confidence, you do not have to manage it alone. Getting the right support early can help you stay active and reduce the risk of falls or further complications.
HWY Physical Therapy offers personalized care for adults 50 and older in Salem, Oregon. Dr. Raj provides one-on-one treatment focused on improving movement, balance, and daily function at the Center 50+ in the Salem City Building.
If you are ready to take the next step, call 971-202-1979 to schedule an appointment. Getting expert guidance now can help protect your mobility and independence for years to come.
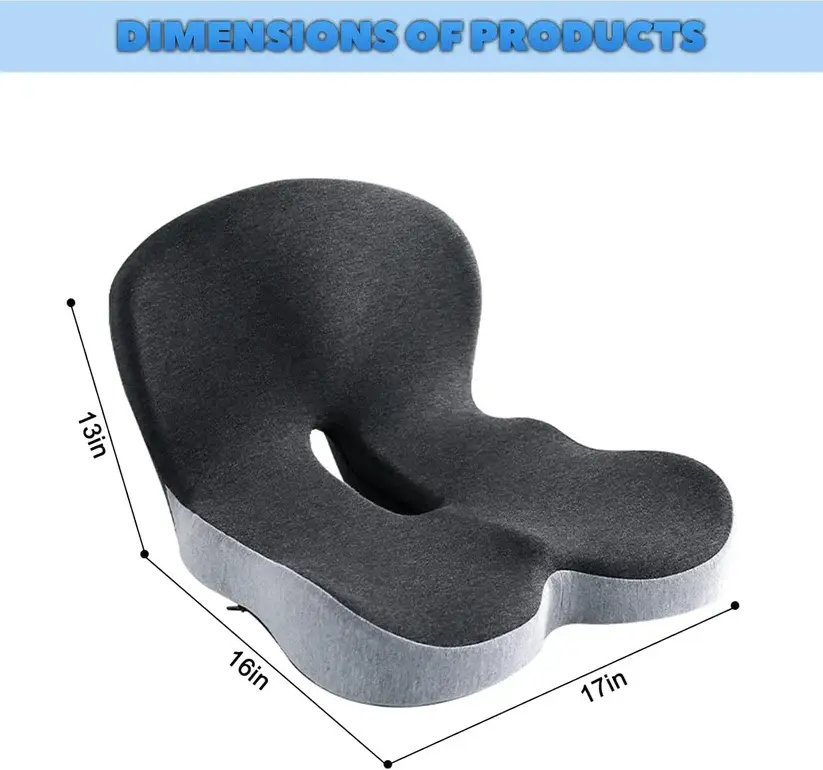
This memory foam one-piece seat cushion with backrest is designed for those who spend extended time seated and value everyday comfort. Created to support both the seat and the back in one continuous form, it transforms ordinary chairs into more inviting, comfortable spaces. Whether used in an office chair or a home seating setup, it delivers a softer, more supported sitting experience.
Foot pain making walking difficult? Learn how physical therapy helps. Get expert care at HWY Physical Therapy Clinic in Salem, OR.
Neuropathy in older adults can affect balance and mobility. Learn symptoms, causes, and treatment options from HWY Physical Therapy Clinic.
Physical therapy for ALS supports mobility, safety, and comfort. Learn how HWY Physical Therapy Clinic in Salem, OR helps patients and caregivers.
Be the first to know about everything latest in physical therapy
.png)
Whether you have questions about enhancing strength, increasing mobility, ensuring home safety, managing pain effectively, or preventing falls, I am here to provide expert guidance.
Limited Time Offer - $25 - Learn More